Ulcerative colitis vs. diverticulitis: Causes, symptoms, risk factors, and complications
 Ulcerative colitis and diverticulitis are two conditions affecting the colon and gastrointestinal system. Nonetheless, their origins, symptoms, and treatments are quite different.
Ulcerative colitis and diverticulitis are two conditions affecting the colon and gastrointestinal system. Nonetheless, their origins, symptoms, and treatments are quite different.
Ulcerative colitis is part of the group of conditions known as inflammatory bowel diseases (IBDs). Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development – although the exact cause is still unknown.
The immune system in IBD patients mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy the perceived enemy. The result of these attacks is chronic inflammation.
Although the exact cause of ulcerative colitis is unknown, genetics and environmental factors are believed to play a role.
Diverticulitis is a condition onset by infection or rupture of diverticula, which are bulges forming in the lower part of the large intestine or colon. The risk of developing diverticula is usually higher for people over 40. Diverticula themselves do not cause many problems, but once the condition progresses into diverticulitis, it can be quite severe, leading to pain, nausea, and changes to bowels.
Mild diverticulitis can be easily treated with a proper diet. However, in cases of reoccurring and severe diverticulitis, surgery may be required.
Ulcerative colitis vs. diverticulitis: U.S. prevalence
The CDC estimated that one to 1.3 million Americans are affected by IBD. Generally, ulcerative colitis is more prevalent in males than females.
Roughly two million people in the U.S. suffer from diverticular disease. Prevalence rate is one in 136, or 0.74 percent. Annually, 300,000 new cases of diverticular disease are diagnosed.
Comparing ulcerative colitis and diverticulitis – signs and symptoms
 Ulcerative colitis symptoms include abdominal pain, increased abdominal sounds, blood stools, diarrhea, fever, rectal pain, weight loss, malnutrition, joint pain and swelling, mouth sores, nausea, vomiting, and skin ulcers.
Ulcerative colitis symptoms include abdominal pain, increased abdominal sounds, blood stools, diarrhea, fever, rectal pain, weight loss, malnutrition, joint pain and swelling, mouth sores, nausea, vomiting, and skin ulcers.
Signs and symptoms of diverticulitis include severe pain that may last for days and takes place in the lower left side of the abdomen, nausea and vomiting, fever, abdominal tenderness, constipation, and in some cases diarrhea (a less common symptom).
Difference between ulcerative colitis and diverticulitis causes
As mentioned, the immune system is suspected to play a role in ulcerative colitis, along with genetics and environmental factors. Certain genes seem to be involved in the development of ulcerative colitis, and having more than four family members with this condition increases your risk of developing it, too. Environmental factors include place of residence, especially because there are higher rates of ulcerative colitis in urban areas, North America, and Western Europe. Air pollution, medications, and certain diets have also been found to be associated with a higher risk of ulcerative colitis.
Weak spots along the bottom of the large intestine can prompt the formation of diverticula. When pressure is added, bulges form. These bulges, or pouches, may protrude through the colon wall. When they burst or get infected, this marks the diagnosis of diverticulitis. It is worth noting that diverticula themselves do not necessarily create symptoms.
Diverticulitis vs. ulcerative colitis: Risk factors and complications
Ulcerative colitis risk factors include having a family history of colitis, being Caucasian, and taking certain medications such as Accutane, Amnesteem, Claravis, or Sotret.
If not well managed, ulcerative colitis can lead to complications, such as severe bleeding, a hole in the colon, severe dehydration, liver disease (although rare), osteoporosis, inflammation of the skin, eyes, joints, mouth sores, increased risk of colon cancer, rapid swelling of the colon, and an increased risk for blood clots.
There are a few factors, aside from age, that can contribute to one’s risk of developing diverticulitis. They are:
- Obesity– being severely overweight may increase the need for surgery as a treatment.
- Smoking– smokers are at higher risk of diverticulitis, compared to non-smokers.
- Lack of exercise– vigorous exercise has been shown to reduce one’s risk of diverticulitis.
- Diet– It is recommended to eat foods that are high in animal fat and low in fiber to lower the risk of developing diverticulitis.
- Certain medications– steroids, opiates, and common over-the-counter pain relievers may all increase your risk of diverticulitis.
Diagnosis for ulcerative colitis and diverticulitis
 Ulcerative colitis diagnosis is made based on a number of tests. Essentially, it is a process of eliminating other conditions. If your doctor suspects an inflammatory bowel issue, they may conduct one or more of the following:
Ulcerative colitis diagnosis is made based on a number of tests. Essentially, it is a process of eliminating other conditions. If your doctor suspects an inflammatory bowel issue, they may conduct one or more of the following:
- Stool tests
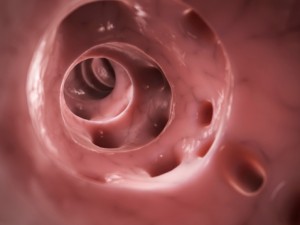
- Endoscopy – a flexible tube is used to examine the small intestine
- Colonoscopy – a flexible tube inserted into the rectum to examine the colon
- Biopsy – an examination of tissue removed from the colon, likely during colonoscopy
- Barium enema – X-rays taken of colon and rectum, using barium to provide contrast.
- Blood tests – to check for low blood count and C-reactive proteins.
If a diagnosis of ulcerative colitis is confirmed, the doctor will discuss the best possible treatment options. Ulcerative colitis treatment can involve drug therapy and surgery. In mild cases, it can simply involve lifestyle changes.
To properly diagnose, diverticulitis your doctor will conduct a physical examination, checking your abdomen and pelvic region. Other tests include blood tests, pregnancy test for women, liver function tests, stool tests, and CT scans, which can help gauge severity of diverticulitis.
Differentiating ulcerative colitis and diverticulitis treatment
In some instances, medications are prescribed to help reduce inflammation associated with ulcerative colitis. Reducing the inflammation can minimize both abdominal cramps and diarrhea. Serious inflammatory bowel disease may require antibiotics or other medications to alter immune function.
When symptoms of ulcerative colitis are severe, hospitalization may be necessary. Oftentimes, severe cases lead to dehydration and malnutrition. Acute symptoms could be a sign of a perforated colon or even cancer. Surgery may be required. There are two surgical options. One, called a protocolectomy, involves removal of the entire colon and rectum. The other, called ileonal anastomosis, involves removal of part of the colon. When proctocolectomy is performed, a surgeon makes a small opening in the abdominal wall to bring the tip of the lower small intestine through the skin’s surface. Waste is then drained through the opening into a bag. With the ileonal anastomosis, feces can still pass through the rectum since the rectum is intact, but the movements will be frequent and watery.
If ulcerative colitis goes undiagnosed and untreated, inflammation can spread, causing problems with other organs and potentially leading to cancer, so proper care and treatment are vital.
Medical treatments for diverticulitis include antibiotics to treat infection, liquid diet to allow bowels to heal, and over-the-counter pain relievers. In complicated cases of diverticulitis, surgery may be required involving primary bowel resection, where the affected part of the intestine is removed, and the rest of it is reconnected. Another option is bowel resection with colostomy if it is impossible to reconnect the colon to the rectum due to inflammation.
If diverticulitis is causing pain, there are home remedies you can try for relief. To reduce muscle cramping caused by diverticulitis, you can apply heat to the abdomen. Meditation, too, may be beneficial in managing the associated pain. Lastly, if you need to opt for a pain reliever, stay away from ibuprofen (Advil), and instead reach for acetaminophen (Tylenol).
There are also some preventative measures you can try to lower your risk of developing diverticulitis.
Regular exercise, in particular, is beneficial for preventing diverticulitis because it helps keep bowels regular. Exercise also works to reduce pressure on the colon. Added pressure on the colon can result in the formation of diverticula.
Fiber, too, is essential. Fiber works to maintain regular bowel movements and helps reduce pressure on the colon. And in this vein, staying hydrated helps. Although fiber can help you stay regular, without enough fluids it can have the opposite effect. Staying hydrated improves bodily functions, so it’s important to drink enough water.
By practicing healthy habits, such as eating a balanced diet, exercising, and not smoking, you can reduce your risk of developing diverticulitis. Although you can’t control aging or turn back the time, you can control these illnesses – and it’s as simple as living well.
-
4 Motives Why You can not Reduce Pounds
So you can not lose fat although youve been following your fat loss
-
Depression in the elderly causes slower response to treatment
Antidepressant therapy may vary among the elderly with late-lif
-
Fire Up Your Fat Burning Machine With These 3 Easy Tips
Do you desire to lose body fat fast, but don’t know where to sta
-
The Romantic 15: Why You Gain Weight When Youre Dating
-
How To Achieve Rapid Weight Loss - Things You Have To Know
Often, losing weight, even on a rapid weight loss program is somethin
-
Information Concerning Weight Loss Products
When it comes to weight loss products there is a huge amount of possib
- DON'T MISS
- Good cholesterol (HDL) levels affected by gut bacteria
- Inner Thigh Exercises
- Losing Weight is an Inside Job
- What Can I Learn About Womens Health And Fitness Training Options?
- How to Really Lose Weight
- The Key To Good Health: Weight Loss And Management
- 8 Tips to Lower Risks of Heart Disease Starting From Young
- A Fitness Plan For The Whole Family
- 8 Major Reasons You Aren’t Shedding Pounds and How to Fix Them!
- Chronic pancreatitis (pancreas inflammation) likely with smoking, alcohol and gene mutation




